Wnt/β-Catenin Signaling in T-Cell Immunity and Cancer Immunotherapy
Recently, at the NY Chemotherapy Foundation symposium, Dr Phil Kantoff from Dana Farber gave a lecture on new therapeutic strategies in prostate cancer. Despite the unsociably early hour (7.30am), the room was almost packed.
While waiting for the session to start, over coffee I had some cheerful banter with some of the oncologists around me. They expressed a keen desire for more tolerable and effective therapies for their mostly elderly patients with prostate cancer, many of whom were too frail or disinterested to really consider chemotherapy once hormone therapies ceased to work.
Several of them were really interested in, but somewhat puzzled about, the recent spate of new data on hormone therapies (abiraterone) and immunotherapy (sipuleucel-T) and how they work, after all, as one pointed out – after a lifetime of treating thousands of patients with chemo and more recently, targeted therapy – getting their heads around new technologies such as vaccines was difficult and challenging to explain to patients in simple language:
“We know that it works, but how does it work? That’s what I’m stuck on.”
Another oncologist wondered why does abiraterone appear to work after failure of docetaxel chemotherapy? He wanted to know if the break from hormone therapy with chemotherapy meant that the androgen receptor (AR) was still driving tumour growth and whether re-treatment with any hormone therapy would actually be beneficial?
Fast forward to Kantoff’s lecture. He covered the basic ground well and also went through the recent trials, including the recent data from ESMO on abiraterone, the NEJM data on MDV3100 and several trials for sipuleucel-T, including the Small et al., (2006) data and the more recent IMPACT trial in asymptomatic and mild symptomatic metastatic castration resistant disease (CRPC) that showed a 4.1 month advantage over placebo, leading to approval by the FDA earlier this year.
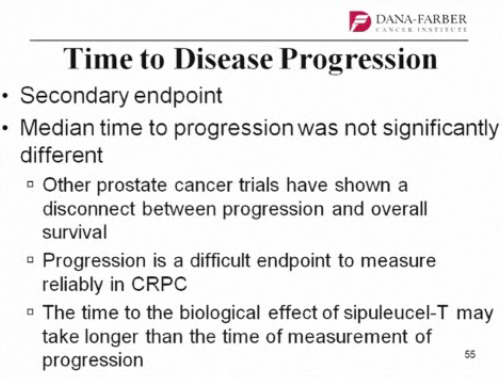
There was some discussion of the survival data, since disease progression, measured as progression-free survival (PFS), may often not be significant, but overall survival (OS) is. Why is this? Kantoff postulated that the time to the biological effect of sipuleucel-T may take longer than the time of measurement of progression (yes, but why?) PFS is also a difficult thing to measure in prostate cancer
The question for me, though, is what is the mechanism behind the delayed biological effect? How can this be explained?
In simple terms, vaccines such as sipuleucel-T rely on stimulating the bodies T-cells to fight the cancer. It doesn’t mean that there will necessarily be any effect on the tumour size, as measured classically by RECIST, but rather the overall impact is inevitably more on immunity effects, which are probably less well understood. Looking through the recent literature, though, I came across a most interesting article in Clinical Cancer Research:
“Wnt ligands are lipid-modified secreted glycoproteins that regulate embryonic development, cell fate specification, and the homeostasis of self-renewing adult tissues. In addition to its well-established role in thymocyte development, recent studies have indicated that Wnt/β-catenin signaling is critical for the differentiation, polarization, and survival of mature T lymphocytes. Here, we describe our current understanding of Wnt signaling in the biology of post-thymic T cells, and discuss how harnessing the Wnt/β-catenin pathway might improve the efficacy of vaccines, T-cell–based therapies, and allogeneic stem cell transplantation for the treatment of patients with cancer.”
We’ve covered Wnt on this blog before, so I’m not going to cover canonical signalling and the delights of Frizzled and Dishevelled in this post, but see here for more background if you’re interested in the biology. Of relevance to this discussion, though, is a quote from the article:
“… the discovery that Wnt/β-catenin signaling is a key regulator of T-cell immunity now raises the possibility that potentiating Wnt signaling could be used to improve cancer therapies through immune-based mechanisms.”
It will be interesting to see if prostate cancer vaccines such as sipuleucel-T actually have an effect on Wnt signalling, thereby explaining the enhanced T-cell effect.
Wnt signalling has also been shown to have a pivotal role in promoting stem cell self-renewal while limiting proliferation and differentiation (see Staal et al., and Fleming et al., 2008 in the references below). Inevitably, the biological effects on immunity can take time to take effect compared to the direct effects of say, DNA methylation or angiogenesis, and this may well explain the delay in efficacy with vaccines. The important thing for men with asymptomatic metastatic prostate cancer is that once it happens, the effect is both prolonged and durable, thereby offering them a new therapy option prior to chemotherapy.
As for the question about re-challenge with existing hormone therapies on the market, I don’t know the answer to that, but it’s a very good question, and perhaps best covered in another blog post unless some of the oncologists reading this have any practical experience to relate?
References:
![]() Gattinoni, L., Ji, Y., & Restifo, N. (2010). Wnt/β-Catenin Signaling in T-Cell Immunity and Cancer Immunotherapy Clinical Cancer Research, 16 (19), 4695-4701 DOI: 10.1158/1078-0432.CCR-10-0356
Gattinoni, L., Ji, Y., & Restifo, N. (2010). Wnt/β-Catenin Signaling in T-Cell Immunity and Cancer Immunotherapy Clinical Cancer Research, 16 (19), 4695-4701 DOI: 10.1158/1078-0432.CCR-10-0356
Staal, F., Luis, T., & Tiemessen, M. (2008). WNT signalling in the immune system: WNT is spreading its wings Nature Reviews Immunology, 8 (8), 581-593 DOI: 10.1038/nri2360
Fleming HE, Janzen V, Lo Celso C, Guo J, Leahy KM, Kronenberg HM, & Scadden DT (2008). Wnt signaling in the niche enforces hematopoietic stem cell quiescence and is necessary to preserve self-renewal in vivo. Cell stem cell, 2 (3), 274-83 PMID: 18371452
One Response to “Wnt/β-Catenin Signaling in T-Cell Immunity and Cancer Immunotherapy”
Interesting post Sally, thanks. I wish I could attend the NY Symposium. Without getting into detail, the answer is yes. For most patients you can recycle some (not all) endocrine therapies. Anti-androgens are the exception but you can try to alternate anti-androgens. For example, I may have someone go from bicalutamide to chemotherapy then after a good response be placed on ketoconazole. When keto fails they may go back to chemo. When chemo fails you can try an alternate anti-androgen or estrogen. And you can repeat this cycle for many patients. The key is understanding how well the patient does on the chemo program and, most importantly, not over-treating with chemo. I do not continue chemo until progression in responders. We get to a good position clinically then consider chemo holidays. Using endocrine therapies here can extend the holidays. Importantly it keeps men sensitive to the prior chemo as well.
Comments are closed.