Reflections of a Medical Oncologist on AACR 2012
While thoughts have already turned to the forthcoming ASCO 2012 meeting and today I am off to AUA 2012 in Atlanta, the annual meeting of the American Association Association for Cancer Research (AACR) last month continues to generate insights.
At AACR I was delighted to meet up with Philippe Aftimos, MD, a Clinical Research Fellow at the Jules Bordet Institute in Brussels, Belgium. Philippe is medical coordinator of the Clinical Research Unit and someone who I met through social media (@aftimosp), so it was a pleasure to meet in person.
I was, therefore, thrilled when Philippe agreed to do a guest blog post about what he thought were the highlights of AACR 2012:
A Medical Oncologist at AACR 2012 in Chicago by Philippe Aftimos, MD
As a medical oncologist with recent interest in clinical research, I attended the AACR annual meeting for the first time in Chicago from March 31st to April 4th 2012.
 At first view, I was impressed by the enormous organization and very large number of participants, which was at least as important as the ASCO annual meeting. However, as a clinician, I only recognized very few familiar faces as the large majority of attendance included basic and translational scientists, as well as representatives of pharma.
At first view, I was impressed by the enormous organization and very large number of participants, which was at least as important as the ASCO annual meeting. However, as a clinician, I only recognized very few familiar faces as the large majority of attendance included basic and translational scientists, as well as representatives of pharma.
Simultaneous sessions took place all over McCormick place and were featured: daily plenary sessions, major symposia, minisymposia, forums, educational sessions, methods workshops, poster sessions, “Current Concepts and Controversies in Organ Site Research” sessions and “Current Concepts and Controversies in Diagnostics, Therapeutics, and Prevention series” sessions. Planning the day’s schedule and navigating between the different sessions was made easy by the well-designed AACR 2012 Annual Meeting app.
My highlights from AACR 2012 can be divided into 3 subjects:
1. Pathways and new drug development
- The PI3K-AKT-mTOR pathway was the subject of multiple sessions. It is mutated in tumors such as breast, lung, ovarian, endometrial carcinomas as well as gliomas. Inhibition of TORC1 has been shown to release inhibition of PI3K. Cancer cells harboring low BIM, a pro-apoptotic Bcl-2 family member, are resistant to PI3K inhibitors. PI3K inhibitors can reverse resistance to anti-EGFR tyrosine kinase inhibitors (TKIs) and the combination with MEK inhibitors is active against K-Ras mutant NSCLC. Selective inhibitors of PI3K isoforms are currently in clinical development. BYL-719 is PI3K alpha inhibitor and has shown tumor shrinkage in the phase 1 setting. It is potent against mutated cells and has anti-angiogenic properties. HER-2 amplification and PIK3CA mutation predict sensitivity while PTEN, B-Raf and K-Ras mutations confer resistance. GSK-2636771 is a selective PI3K beta inhibitor potentially inducing synthetic lethality in PTEN deficient mice. Hyperglycemia and hyperinsulinemia are class adverse events of PI3K inhibitors but are seldom seen with GSK-2636771.
- ABT-199 is a Bcl-2 inhibitor in phase 1 development with very promising activity starting from the first cohort (starting dose) of chronic lymphocytic leukemia patients. It has also shown synergy when combined with rituximab or combination chemotherapy. Activity is correlated to Bcl-2 expression and specific targeting of Bcl-2 reduces the incidence of thrombocytopenia.
- With the discovery of new chemotherapy agents in the treatment of castrate-resistant prostate cancer, interest in anti-hormonal treatments has been renewed. AZD-3514 is a first in class selective androgen receptor downregulator (SARD). It targets the androgen receptor in the nucleus and is currently in phase 1 development.
- PD-0332991 is a highly selective inhibitor of CDK4/CDK6 resulting in potent G1 arrest, especially in Rb positive tumors. It showed activity in phase 1 trials with stable disease in breast cancer and liposarcoma. The most impressive results were in the treatment of mantle cell lymphoma with 1 CR in one patient still on-study for 2 years, 2 PR with one patient on study for 30 months and 7 SD out of 16 patients. Main DLT was neutropenia. Thrombocytopenia was also a limiting factor.
2. Immune therapy
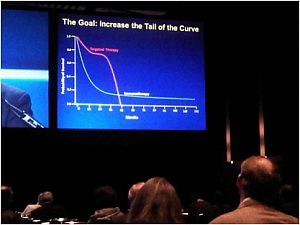 The goal is to increase the tail of the curve in the photograph in the right. The approval of ipilimumab in the treatment of metastatic melanoma has inaugurated the new era of anti-cancer immune therapies.
The goal is to increase the tail of the curve in the photograph in the right. The approval of ipilimumab in the treatment of metastatic melanoma has inaugurated the new era of anti-cancer immune therapies.
They were very much put in the spotlight at AACR 2012 with a plenary session entitled: Immune Therapies: The Future Is Now. Highlights included: adoptive T-cell therapy, recombinant pox-viral vaccines, intra-tumor injection of vaccines, combination of vaccines and targeted agents in the treatment of melanoma. Characteristics of therapeutic vaccines are: minimal toxicity, indirect effects on tumors, delayed responses that increase over time. Administration in the early course of disease may be better and overall survival is usually the endpoint of clinical trials.
Agents that most caught my attention were monoclonal antibodies targeting the Programmed Death-1 (PD-1) T cell co-receptor and its ligand, B7-H1/PD-L1. Durable responses have been seen, often long-lasting off-therapy. Overall response rates as high as 30% have been demonstrated in renal cell carcinoma and melanoma. Tumor shrinkage was also seen in non-immunogenic cancers such as non-small cell lung cancer. Strong endogenous anti-tumor immune response upregulates PD-L1. For week endogenous anti-tumor immune response, combinations with epigenetic therapies may be key. Agents such as azacytidine can create an inflammatory response. Search for biomarkers such as PD-L1 expression and tumor-infiltrating lymphocytes is ongoing. This reference further explains this pathway: Topalian SL, Drake CG, Pardoll DM. Curr Opin Immunol. 2012 Apr;24(2):207-12.
3. Challenges for the future
With many clinical trials yielding negative results, the necessity for “smarter” trials has become evident. Trials of the future should be biomarker-stratified, enriched and adaptive. Histology-independent, aberration-specific trials should also be considered while being aware of different degrees of functionality and sensitivity of mutations. Combinations of targeted agents are the backbone of recent clinical trials and scientific rationle should be strong:
- Supportive and confirmed in vivo and preclinical data
- Suitable animal toxicity
- Predictable biomarkers
- Delivery to patients: number of pills, …
2 challenges remain:
- Cooperation between different pharmaceutical patients developing the drugs of the combination
- Regulatory-acceptance of mutation-based trials as well as regulations for targeted agents combinations
The session tackling the last issue deserved to feature as a plenary session. A very large crowd attended it with many participants finally sitting on the floor or leaning on walls.
Finally, the 2012 AACR Annual Meeting was yet another example of the rapid development and influence of social media with many scientists, clinicians and pharma representatives tweeting the information live, sharing their opinions, and interacting together.
Bio: Philippe Aftimos, MD
Medical Oncologist, graduate of Saint Joseph University in Beirut, Lebanon and the Free University of Brussels, Belgium. Trained: MD Anderson Cancer Center (Houston, Texas), Memorial Sloan-Kettering Cancer Center (New York City, New York) and Institut Gustave Roussy (Paris, France).
Currently, medical coordinator of the Clinical Research Unit at Institut Jules Bordet Cancer Centre in Brussels, Belgium, investigator for multiple clinical trials. My main interests are new drug development, phase 1 trials and breast cancer.
One Response to “Reflections of a Medical Oncologist on AACR 2012”
I enjoyed reading this post. I am not a doctor but I am a researcher. In my continued fight against cancer, research has proven my best defense. I have been in a phase I trial of pazopanib with topotecan for over 2 years with no progression of disease. Unil today. Today I learned that the left periaorta lymph node is 2 mm larger (at 8mm) and that the biopsy revealed cancer cells. I am currently looking for a promising trial to switch to. I am thinking that perhaps if we take the lymph node out with a gamma knife first it would be most helpful. The cancer is recurrent uterine cancer. I have done radiation twice, first with carboplatin/taxol and next with adriamycin(sp??). The cancer recurred immediately following the end of each of those treatments. I have done very well with the pazopanib but that, evidently, is at an end. If anyone reading this post has any suggestions as to the next best course of treatment I would be most appreciative. I realize that no one has an absolute answer but it would surely help me to choose the best course if I had the recommendation of someone more knowledgeable than I am. Thank you so much. Valerie
Comments are closed.