Clinical implications of breast cancer stem cells
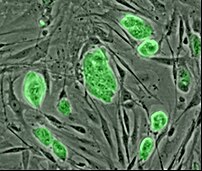
Image via Wikipedia
The cancer stem cell hypothesis proposes that tumours arise in either
normal stem or progenitor cells through the disregulation of
self-renewal processes. These 'cancer stem cells'
inevitably display resistance to chemotherapeutic agents and so relapse or recurrence may occur if they are not wiped out.
Historically, chemotherapy has been used to attack the cancer cells and shrink the tumour. New potential agents for targeting stem cells range from antibodies that form complexes with antigens on the surface of the cancer cell to small molecules that have been engineered to block key enzyme pathways. The interaction of the antibody or drug with its target inhibits pathways that are essential for cell proliferation or metastasis or activates pathways that culminate in cell death (apoptosis). These targets are usually specific for, or over-expressed, in cancer cells.
Fortunately, the new targeted agents generally have fewer side effects than most conventional chemotherapeutic agents and when the targeted agents are combined with single-agent chemotherapy, toxicity is usually only minimally increased. Combinations of targeted and conventional chemotherapeutic agents may improve the response to treatment without a major increase in side effects.
If we consider the goal is to improve the chance for a cure, these new treatments appear worth the expenditure. However, when the goal is to improve the quality of life or delay the time to disease progression by only a few weeks or months, often in the case with treatments for metastatic cancer, it is less clear whether the health care system can or should bear the financial burden of doing so. Further research is likely to evolve using biomarkers to determine who would most likely benefit from receiving individual therapies, thereby conserving valuable resources and matching patients to treatments most likely to work for their particular situation. This would be a win-win approach all around.
