Following last weeks post on the phase III clinical data for tivozanib in advanced renal cell cancer (RCC), I thought it would be useful to provide an update on AVEO’s biomarker program.
I’m very excited about the work they are doing in this area and have been following them keenly since they first presented their initial work on myeloid cells in RCC at the AACR diagnostic conference back in 2010. Since then, other companies have also published work in this field, including Regeneron, who also noticed the presence of myeloid cells in their work with aflibercept in glioblastoma.
Biomarkers have been very much a bête noire in angiogenesis research – we know that some patients respond well to therapy, but others do poorly and may actually be worse off. The challenge has been finding a way to link biology with response in order to improve patient selection. Genentech/Roche have laudably spent millions in their quest for biomarkers with bevacizumab (Avastin), with researchers clearly very frustrated at the confounding data presented at the 2011 ECCO meeting in Stockholm. Clearly, we have a long way to go in this field.

Murray Robinson, Courtesy of AVEO
Last week I caught up with AVEO’s Murray Robinson (who is the Special Advisor to the CEO), to discuss the progress they are making on the biomarker front.
The recent ASCO GU meeting in Orlando highlighted very interesting data on a new biomarker they are researching, which involves a hypoxia gene signature in RCC (PDF download).
While this data is still preliminary at the moment, it is being tested prospectively in some ongoing trials in both renal and breast cancers. Readouts are expected by the end of this year and may reveal some interesting findings.
PSB: Does the hypoxia biomarker in your poster at ASCO GU connect with the myeloid biomarker you presented back in Denver at AACR, or is this completely different?
Murray Robinson: This is one is independent of that, completely different, although as you can imagine we are looking at the myeloid biology in this same dataset. To put that to rest, we ran into some technical details, technical challenges on that. Remember when you are doing these trials, you only get the material you get, and you don’t always get the quality, and can’t go back and recut it.
We are really looking forward for the marker in this paper as well as that that myeloid work, to an ongoing study of a 100 patients mostly in the US, RCC – BATON (Biomarker Assessment of Tivozanib ONcology) study and we will get to take another look at this hypoxia biomarker, the myeloid biomarker and a few others that we are looking at. That study will mature soon, we are expecting probably sometime later this year.
PSB: Are these two biomarkers going to be practical in the future for community oncologists to use or is it going to be something that is a research tool do you think?
All of us are now applying high resolution molecular analysis to all of the tumors, all the TCGA work, whole genome transcriptome on things. As the field has done that, we have all been amazed and enlightened by the complexity within what the field used to call a single genotype.
We are all recognizing there are many molecular subsets. This of course was first elucidated 10 years ago in breast cancer. In breast cancer we are very comfortable with these idea, it’s not breast cancer, it’s ER+, or HER2 amplified or triple negative. And of course treatment assignment can be based on that, and we are even further refining those subsets. We haven’t that kind of resolution until recently with many of the other tumor types.
Let’s turn to renal cell carcinoma, (RCC) which is the subject of this work. We in the field have long considered clear cell renal carcinoma, which is 85% of RCC, to be a tumor type. However, as the field has begun to sequence and do profiling on many of these tumors, we have begun to recognize that it is in fact more complex than that.
In our poster, we first cited some great pioneering work by Dr Kim Rathmell down at UNC Chapel Hill where she really was one of the first to take a look at these subtypes of clear cell, and has reported now, and we excerpted one of her figures from a recent paper of hers on our poster. And she sees three major subtypes of clear cell kidney cancer. Two of those subtypes she has talked about before, and we won’t spend much more time talking today. They don’t seem to differentiate for a number of key biological features. A third type she has identified, and we also independently identified, is the subject of this work.
What we, and others, have recognized is that there are new, previously underappreciated, subtypes of clear cell carcinoma. We focused on this one novel subtype, which Kim called Cluster 3, and we then applied some of our own bioinformatics platform to this, in which we have comprehensively charaterized tumors for key robust signatures.
We applied those key robust signatures that usually represent biology to this third tumor type. We saw that there were a number of key features in which these tumors varied, this is about 15% of clear cell RCC, so it is a relatively small subset. We noticed in particular that one of the dominant differentiating features of this tumor was the expression of its hypoxia responsive genes.
We recognize there’s a different tumor type here, and that the tumor type is now low for a large signature that we have had for hypoxia, and we of course are thinking translationally, and in terms of molecular diagnostics as well. We optimized to reduce that hypoxia gene signature to a nine gene signature and we optimized the ability to measure those genes often using single sections from clinical paraffin embedded material.
We are absolutely thinking about this biology and are looking toward to the development of a simple diagnostic test, if that were warranted.
We looked at that nine gene signature, quantified it then looked at its impact on response to tivozanib as well as sorafenib.
PSB: My understanding from looking at your poster in this particular subset with the hypoxic element is that some patients did better in response to tivozanib than others?
Murray Robinson: That is the observation that we made.
Our interest in looking at hypoxia in tivozanib is that hypoxia as we showed in one of our figures, that signature relates to the over-expresssion of key VEGF ligands, VEGFA, PLGF and VEGFC.
One hypothesis that we generated from these observations is that when the VEGF pathway is deregulated or overactive as it is in most of clear cell, then you are more likely to respond to a selective, potent VEGF pathway inhibitor like tivozanib. Conversely, then if you find a subtype that is not, the hypothesis is that it would not respond well.
We tested that in the study, and with the important caveat that we had 69 samples out of the total trial of 517 patients, then we looked at this subtype. Well, we predicted the subtype would represent about 15% of the total, so we went form 69 down to about 30 samples, then 15% of those I think we ended up with 4 of the low subtype in both [arms]. We all recognize those are pretty small numbers. We are really looking forward to the second study I mentioned to you.
PSB: You will still have to validate the results in a larger sample?
Murray Robinson: We think that would be prudent. We think it is difficult to make much out of 4 samples, however that is the amount that would be predicted. It is consistent with all the work that we have done previously. We are also certainly pleased that those 4 patients did not perform well on tivozanib, whereas in the remaining 85% of those patients, those patients did very well.
In fact median PFS of the high patients, representing 85% of the study population, was 18.3 months, which is very respectable progression free survival.
PSB: In other words you have a very good way upfront to potentially predict up front which patients might do well on tivozanib?
Murray Robinson: That was the hypothesis going into this, this was a prospectively designed hypothesis that we wrote up. It was not exploratory.
There is another point here that we’re pretty excited about. One thing we know about the field, that we didn’t 10 years ago, is that despite the original enthusiasm around the VEGF pathway as being a key angiogenesis inhibitor pathway, we all know the large amount of clinical data over the last 10 years with different VEGF pathway inhibitors has been disappointing.
I think there has been a lot of disappointment about the expectations about the VEGF inhibitors versus their performance. The VEGF pathway inhibitors are working, there are a number of indications there, but it certainly hasn’t been that universal broad-acting, cytotoxic agent that we all thought it was, would have been back in 1999.
The bigger question is can we use an understanding of the biology, an understanding of gene signatures, to better select patients in other indications? What we showed in this paper is that 85% of these patients have this VEGF deregulation signature and that is consistent with the fact that clear cell carcinoma actually exhibits robust single agent response to tivozanib and activity with other VEGF type agents.
We really are interested with the signature in expanding and using this as a biomarker outside of clear cell carcinoma, and we have now have done that. Those studies are in progress.
We did a survey of this hypoxia signature across multiple tumor types and made an observation that we are pretty excited about. That is, we found that the hypoxic signature is not as prevalent in those tumor types as it is in clear cell.
We did find that it was present in subsets of tumor types, and we particularly noted that in triple negative breast cancer (TNBC), the hypoxia gene signature is high in a high proportion of triple negative breast cancer.
That is interesting because there is some anecdotal or retrospective clinical data that suggests that VEGF pathway inhibitor agents may work a little bit better in triple negative breast cancer, a challenging tumor type with high unmet medical need.
That observation led to us starting a new phase 2 trial in breast cancer, the BATON-breast study that we started a few months ago. In that study, we will be looking at triple negative breast cancer and we are looking at a randomized phase 2, and we are looking at paclitaxel versus paclitaxel plus tivozanib. In that study we will be measuring the hypoxia biomarker signature.
We have started that and are planning on using a specific assay to look at those patients.
PSB: And finally, for the prospective renal trial with biomarkers when do you expect that to read out, is it anytime soon?
Murray Robinson: I would expect to look for that around the end of the year, recognizing that we don’t know when that’s going to mature, but second half of the year that is when we are expecting. We are looking forward to those results.
We think that there is a strong hypothesis for this and we are pleased in the TIV0-1 study that we saw data consistent with the hypothesis.
Some personal thoughts and additional insights…
Before anyone gets in too much of a tizzy, note that the data reported at ASCO GU are preliminary findings in a small sample size with only a few (n=4) hypoxia low patients, as Dr Robinson fairly pointed out. They need to be validated prospectively in a randomised controlled study to ensure that the initial findings are real and not a fluke. The good news, however, is that the consistent lack of response in these patients enabled the hypothesis to be tested further in new trials. It’s certainly a concept that worth testing.
We have known, or suspect, that VEGF inhibitors work in conditions of tumour hypoxia, but this is the first time I can recall anyone connecting the hypothesis to clinical response. Assuming that the findings can be validated in the prospective trials – and a commercial assay developed in the future – then the ability to select patients with RCC who are more likely to respond to a VEGF inhibitor such as tivozanib would be most welcome.
Would other VEGF inhibitors need to show the same effect or would a class effect be assumed? In my book, you can’t always assume that one biomarker for one drug will always translate to others without data. In this study a significant effect was seen for tivozanib but not sorafenib based on the hypoxia biomarker. We don’t know what the impact is with other VEGF inhibitors such as sunitinib, pazopanib, bevacizumab and axitinib. It will be most interesting to see what happens here, as the hypoxia biomarker made be a differentiating factor for tivozanib in the future.
The upside for a VEGF inhibitor in TNBC is potentially huge, much bigger than RCC. What would drive this element though is not only positive data but also a way to predict and select which patients are more likely to respond. Essentially, if the data is positive, it may well redefine a subset of the disease, much in the same way that CD117 (KIT) enabled GIST patients to be differentiated from other types of soft tissue sarcomas. When you can do that, it makes matching treatment to patients a whole lot easier for clinicians and pathologists.

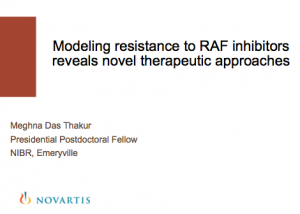 That’s what a young Novartis Postdoctoral fellow from NIBR, Meghna Das Thakur, did. She asked critical questions and attempted to answer them in a series of elegant experiments with mice as well as retrospectively test the concept in patient data. The cool thing is that while many of the oral sessions were taken up by the Major League researchers is that it’s also nice to see up and coming young scientists present some nicely done research.
That’s what a young Novartis Postdoctoral fellow from NIBR, Meghna Das Thakur, did. She asked critical questions and attempted to answer them in a series of elegant experiments with mice as well as retrospectively test the concept in patient data. The cool thing is that while many of the oral sessions were taken up by the Major League researchers is that it’s also nice to see up and coming young scientists present some nicely done research. With around 6,000 posters and many oral presentations from leading researchers, there is usually some interesting early data coming out from AACR. This year was no exception. My pile of poster handouts is over 6” thick with more already coming in my email! My fervent wish for next year is that more scientists take to the QR code method of sharing their posters – aside from being green and saving trees, it’s also considerably easier on the back! Another welcome development would be putting the posters online for later download as many of the European meetings already do.
With around 6,000 posters and many oral presentations from leading researchers, there is usually some interesting early data coming out from AACR. This year was no exception. My pile of poster handouts is over 6” thick with more already coming in my email! My fervent wish for next year is that more scientists take to the QR code method of sharing their posters – aside from being green and saving trees, it’s also considerably easier on the back! Another welcome development would be putting the posters online for later download as many of the European meetings already do.

