Late last week saw an incredible amount of noise in the media over the startling news that three patients with chronic lymphocytic leukemia (CLL) had responded well to an experimental gene therapy that aimed to boost T cells to fight a particular type of leukemia, some of it, unfortunately, bordering on near hysterical hype, such as MSNBC’s article entitled:
“New leukemia treatment exceeds ‘wildest expectations'”
Ugh. There were others in similar vein, mostly derived from the AP and Reuters press releases. Quite frankly, with a headline like that I was expecting something more substantial and robust than three patients.
The most measured story I saw came from NPR Shots, who took a more rational and thoughtful approach to the publications in New England Journal of Medicine and Science and Translational Medicine.
Gary Schwitzer also did a nice review of some of the commentary that emanated from the health media outlets as well as a well thought out longer piece.
It was clear though, that some of my medical and science friends were rather disappointed by the rather breathless nature of the general media reporting. There is something really icky about raising peoples hopes based on very minimal data. Part of this is due to journalists and editors with attention grabbing headlines, presumably because that’s what drives traffic, but also a noticeable lack of rigour or critical thinking in reviewing the situation in depth.
Let’s take a look at the disease in more detail first.
CLL is well known to be a disease of the elderly, with a median age around 63-65 years. It’s an indolent immune-sensitive cancer and treatment is largely based on a series of immunotherapies, either alone or in combination, such as fludarabine, rituximab, bendamustine, pentostatin and alemtuzumab, for example. Not one of the media reports I read looked at how refractory these patients (only a small sample of n=3) really were or what their prognosis was. It is well known that patients can live normal lives between treatments until relapse, when another treatment is initiated. This process can go on for several years but eventually, they run out of options as these patients did.
What do we know about the patients?
Looking at the actual data reported from the two journals, we find some interesting nuggets about their prior immunotherapy treatment and karyotypes:
- The NEJM article is a single case report on one patient who had previously received FR (twice, for 2 and 4 cycles), BR (1 cycle), B (3 cycles) and alemtuzumab. He was found to have a 17p del with TP53 involvement, which has a known poor prognosis.
- All three patients had received both bendamustine and alemtuzumab (in different lines of treatment).
- Not all of the patients appear to have received prior fludarabine, which is surprising given that it is largely considered to be the standard of care, either as fludarabine-cytoxan-ritiximab (FCR) or fludarabine-rituximab (FR). (Note: The patient who achieved a PR rather than CR did not apear to receive prior fludarabine).
- Two of the patients had a 17p deletion (with p53 involvement), the other had a normal karyotype. The latter generally has a better prognosis.
- No indication of what might be expected without treatment in terms of the time elapsed after the last therapy is feasible without a comparative trial, so evaluating the effects of the gene therapy versus a control group will be needed going forward.
- None of the patients appear to have received a prior bone marrow transplant, which while potentially curative in about half of patients, is not without its complications such as a 20% chance of mortality from the procedure itself.
- All of the patients experienced some degree of tumour lysis with fevers, chills, nausea and fever, which occurs when many cancer cells die at once.
The tumour lysis reported in the patients is the most encouraging signal that the gene therapy was working effectively.
What did the researchers do?
Porter et al., (2011) described the idea behind the gene therapy in the NEJM article:
“In most cancers, tumor-specific antigens for targeting are not well defined, but in B-cell neoplasms, CD19 is an attractive target. Expression of CD19 is restricted to normal and malignant B cells and B-cell precursors”
This knowledge provided an opportunity to create a targeted gene therapy and test it in a pilot proof of concept study in a small sample size (n=3). Patients cells were removed and then a personalised gene therapy was created:
“We designed a self-inactivating lentiviral vector (GeMCRIS 0607-793), which was subjected to preclinical safety testing, as reported previously.”
In plain English, the lentivirus vector encodes an antibody-like protein known as a chimeric antigen receptor (CAR), which is expressed on the surface of T cells and was designed to bind to the CD19 protein used as the target.
The U. Penn press release described the rationale behind the targeted therapy further:
“Once the T cells start expressing the CAR, they focus all of their killing activity on cells that express CD19, which includes CLL tumor cells and normal B cells.
All of the other cells in the patient that do not express CD19 are ignored by the modified T cells, which limits side effects typically experienced during standard therapies.”
What results were seen?
Two patients (one normal karyotype, one with a 17p TP53 del) were seen to have a complete response (CR) of 10 and 11 months each.
A third patient with a 17p TP53 del was adjudged to have a partial response (PR) of 7 months.
These results were fairly encouraging and offer a good proof of concept that the gene therapy is viable in CLL patients. They also justify pursuing the gene therapy approach in larger scale clinical trials.
What do these data really mean?
Very little, other than an initial proof of concept, based on such a small sample size, but it does give some encouragement to move forward with a broader program to validate the findings. At present, there is no doubt that people who have CLL with 17p and TP53 deletions tend to experience shorter remissions after standard therapies, so a new option that can be evaluated in clinical trials is an encouraging and welcome sign of some progress in this area.
Overall, while encouraging, these results are best described as ‘promising, but very early indeed’ – a lot more data will need to collected from randomised controlled trials before we see whether we really have a viable new therapy for people with CLL. To suggest anything else is hype over hope at this stage and that does a great disservice to people with the disease.
Far too many agents fail between initial proof of concept to actually filing for Health Authority approval based on phase II or III data to raise hopes unnecessarily. In fact, given more therapies fail in R&D than make it market, we would best remember that before we call anything the new ‘breakthrough’ or ‘killer therapy.’
I’m looking forward to seeing the gene therapy program develop further in larger randomised clinical trials, hopefully without excessive hype.
In an editorial in the NEJM, Urba and Longo (2011) urged some caution:
“Only with the more widespread clinical use of chimeric antigen–receptor T cells will we learn whether the results reported by Porter et al. reflect an authentic advance toward a clinically applicable and effective therapy or yet another promising lead that runs into a barrier that cannot be easily overcome.”
I couldn’t agree more with those sentiments.
Still, on a much lighter note, XKCD came to the rescue with this awesome cartoon to brighten up a dull grey morning:
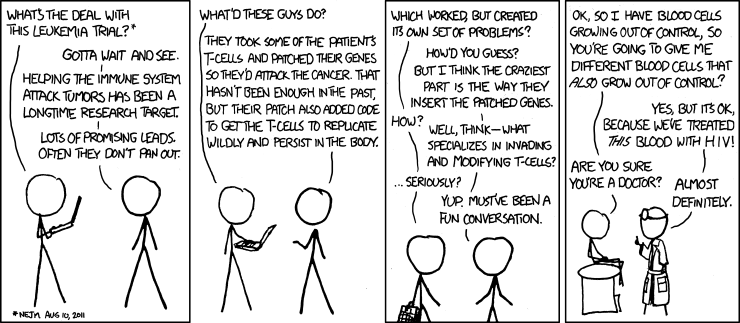
Source: XKCD
References:
 Porter, D., Levine, B., Kalos, M., Bagg, A., & June, C. (2011). Chimeric Antigen Receptor–Modified T Cells in Chronic Lymphoid Leukemia New England Journal of Medicine DOI: 10.1056/NEJMoa1103849
Porter, D., Levine, B., Kalos, M., Bagg, A., & June, C. (2011). Chimeric Antigen Receptor–Modified T Cells in Chronic Lymphoid Leukemia New England Journal of Medicine DOI: 10.1056/NEJMoa1103849
Kalos, M., Levine, B., Porter, D., Katz, S., Grupp, S., Bagg, A., & June, C. (2011). T Cells with Chimeric Antigen Receptors Have Potent Antitumor Effects and Can Establish Memory in Patients with Advanced Leukemia Science Translational Medicine, 3 (95), 95-95 DOI: 10.1126/scitranslmed.3002842
Urba, W., & Longo, D. (2011). Redirecting T Cells New England Journal of Medicine DOI: 10.1056/NEJMe1106965



 Last month, a critical paper was published in
Last month, a critical paper was published in